Feature Story
Health Center Today, March 10, 2011
Using Stem Cells to Regrow Muscle and Bone
By Christine Buckley
David Goldhamer, associate professor of molecular and cell biology.
Photos by Daniel Buttrey
Among the most debilitating of diseases are degenerative ones, in which a person’s health slowly declines over time. And some of the worst of these diseases involve the deterioration of muscle or bone.
Molecular biologist David Goldhamer is using stem cell technology to try to put a stop to these diseases and related injuries.
Goldhamer, an associate professor of molecular and cell biology in the College of Liberal Arts and Sciences and director of the Center for Regenerative Biology, is using genetic techniques in mice to understand the repair of muscle and bone in diseased and damaged tissues. He and his colleagues have recently been awarded grants by the Muscular Dystrophy Association and the U.S. Department of Defense to study Duchenne’s Muscular Dystrophy; a rare bone disease (Fibrodysplasia ossificans progressiva); and the recovery of wounded soldiers returning from war.
The Role of Satellite Cells
Last month, Goldhamer was awarded $375,000 over three years from the Muscular Dystrophy Association to investigate muscle stem cells, called satellite cells, and their role in regenerating muscle tissue that is damaged by injury or disease. These cells are positioned just outside muscle fibers and are responsible for the repair and growth of muscle cells.
When muscle is injured, he says, these cells start dividing, and participate in the process of muscle regeneration. In his laboratory, Goldhamer uses genetic marking methods to understand how the cells work: “We want to know: How do satellite cells get programmed for muscle regeneration? What are the cellular and molecular underpinnings? How is it genetically controlled?”
One of the histological hallmarks of advanced stages of Duchenne’s Muscular Dystrophy, he continues, is the abnormal accumulation of connective tissue and fat cells inside muscles. These foreign cells destabilize the muscles surrounding them, creating a decrease in muscle strength. Goldhamer wants to know whether altered satellite cell programming or other stem cells in muscle tissue are responsible for these pathological changes.

Doctoral student Michael Wosczyna and Goldhamer examine a tissue sample in their lab
In young patients, the satellite cells create new muscle as it disappears, keeping the patient relatively strong. But as the patient ages, the cells can no longer keep up with the disease.
Learning about how these satellite cells function will also help Goldhamer understand how they might be altered to help combat the disease. For example, stem cell therapies have shown that when these cells are injected into muscle tissue, they can contribute to new muscle formation. However, the cells are limited to a small area around the site of injection, and most of the cells die.
Goldhamer notes that the cells will survive longer after injection if they have a particular favorable mutation, which could lead to development of more comprehensive cell therapies.
“If they’re going to be used in patients, there’s a problem of scale,” he says. “Unless the survival rate and migration improves, then they won’t be useful in therapies.”
Preventing Unwanted Bone Formation

Michael Wosczyna studies muscle tissue through a microscope.
Another facet of Goldhamer’s research involves the rare bone disease Fibrodysplasia ossificans progressiva, or FOP. Caused by a deleterious genetic mutation, the disease causes bone cells to be created within muscles. This formation of bone in inappropriate places, known as heterotopic ossification, is progressive throughout a patient’s life, resulting in devastating effects on health, life expectancy, and quality of life.
Along with principal investigator David Rowe of the UConn Health Center and a team of other researchers, Goldhamer is involved in an upcoming project that will be supported by the Department of Defense. His role in this research will be to study the process of heterotopic ossification.
The Department of Defense is interested in funding this research, he says, because it also has applications for helping injured war veterans.
“Heterotopic ossification is a common occurrence in soldiers who have suffered a blast injury to the extremities,” he says. “They grow bone in their soft tissue, and it’s a significant complication that can have a profound effect on muscle structure, impede rehabilitation, and affect the extent of functional recovery.”
Yet the cause of this ossification has remained unknown. Goldhamer and his graduate students, Michael Wosczyna and Arpita Biswas, recently identified a cell that could be part of the pathological response that creates bone. He and his colleagues will now try to characterize this cell to determine whether it could be prevented from creating bone in muscle – and, potentially, be used in bone repair.
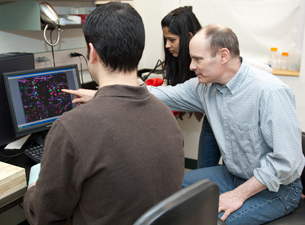
Doctoral students Michael Wosczyna and Arpita Biswas look on, as Goldhamer points out muscle cells in a microscope image.
As promising as these developments could be, Goldhamer says they also create challenges.
“Aggressive repairs of bone in soldiers could result in heterotopic ossification of surrounding musculature,” he says. “Any reparative strategy will have to be precise and localized.”
Although he’s been interested in regenerative biology since he was a graduate student studying limb regeneration in salamanders, Goldhamer says his work was put into perspective when he first interacted with people who have FOP, at a conference that brought together both scientists and patients who have the disease.
“It brought home the significance of my work in a profound way,” he says.


